By Ben Mauro
Shoulder instability – is it ‘normal’ or ‘okay’ for my shoulder to dislocate or give way easily?
The shoulder is one of the most mobile joints in the body and allow us to move our upper limb in many directions and in various positions. With this abundance of MOBILITY, it is then vital that there is an appropriate amount of STABILITY to keep the shoulder safe and healthy. Unfortunately, shoulder dislocations occur fairly regularly (approximately 2-8% of the general population) but what is more alarming is the frequency at which shoulder instability reoccurs.
Our shoulder is made up of 4 main joints:
- Glenohumeral joint
- Acromio-clavicular joint
- Sterno-clavicular joint
- Scapulo-thoracic joint
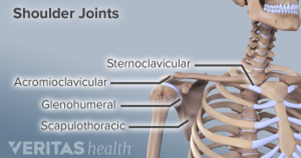
The most common site of instability comes from the Glenohumeral joint commonly referred to as the ‘ball and socket’ joint of the shoulder. A dislocation occurs when the humeral head ‘the ball’ is disturbed from glenoid fossa ‘the socket’. Usually this occurs in an anterior direction – up to 95% of shoulder dislocations happen anteriorly – but it can occur inferiorly or posteriorly too.
There are also 3 types of shoulder instability:
- Traumatic – a direct impact to the shoulder causing it to dislocate
- Atraumatic – a force causing dislocation from a quick or large direction movement of the arm
- Non-Traumatic – dislocation from a positional posture of the arm where it feels it will give way or pop out without much force
If we now look at reoccurring dislocations, the biggest statistical feature of reoccurring dislocations is your age of the initial dislocation. If you were under 20 years of age when you first dislocated your shoulder, you are more likely to dislocate it again and multiple times throughout your lifespan – between 66-100% likely (depending on the study you look at). Where if you are 40 years or older when you first dislocated your shoulder, it’s only 16% likely for this to occur again.
With the shoulder being a very mobile joint, an injury such as a dislocation can impact the ability of the surrounding tissue to keep the shoulder safely stable and healthy to perform day to day tasks. It is therefore VERY IMPORTANT to get your shoulder seen to by a physiotherapist when you dislocate your shoulder for the first time to help prevent these reoccurring dislocations.
So, you’re now up to speed on the different types of dislocation and what a dislocation actually is! Now let’s refer back to the initial question – is it normal for shoulders to easily dislocate? As the statistics show it can be common, but it all comes down to context. If your shoulder is holding you back from doing what you want to do with it, then it should be seen to. An example of this could be a labourer who must modify their work due to the feeling of giving way, or someone who’s unable to hangout the washing because of pain overhead, or a footballer who has reoccurring dislocations to the point of needing to quit the sport. In these situations, I would say it is not OK or NORMAL for you to continue to put up with this. These are the cases that are often overlooked for months and sometimes even years before anything is done about it. The purpose of this blog is to bring awareness that something can be done… but where do you start?
In these ongoing persistent unstable shoulder cases, we believe it should start with a physiotherapist and a detailed history. Going through a detailed history and coming up with ideal goals and activities that you would like to achieve should be priority number 1! Imaging, assessments of strength and function are also important, but how you perceive your shoulder health is also vital for best outcomes. This may be a quick questionnaire or some details discussion about your shoulder health, but it all starts with detailed discussion. Some questions may consist of:
- When did you first dislocate your shoulder?
- How many times in the last 12 months have you dislocated or subluxed you shoulder?
- Are there daily activities you alter or avoid because your shoulder feels unstable or going to ‘give way’?
From this discussion we can then set up a more realistic pathway for best outcome. This may include daily strength exercises to gain better strength and control in positions of instability. It may include further diagnostic imaging to see what structures could be the cause of the shoulder’s instability, or in some cases it may require further discussion and referral onto a specialist to seek advice on whether a surgical intervention is necessary. Everyone is different and every outcome may vary depending on the information gathered, but having a start point begins our journey to set you up on a pathway to improve your shoulder for the long term!