Today (20th Oct) is world osteoporosis day. This brings attention to a condition that is a contributor to hundreds of thousands of hospital admissions each year for fractures. In 2012, 67% of South Australians over 50 years of age were recorded to have osteoporosis, or osteopenia (weakening of the bones, and precursor to osteoporosis). This number is expected to continue increasing.
As someone who regularly sees the impact of osteoporosis and osteoporotic fractures on the lives of adults, and particularly older adults in the hospital setting (where I spend my other days of the week when I am not at Connect Healthcare!), supporting our bone health with good lifestyle habits really is something I consider a priority across the lifespan. Whether you are early in your adult years, somewhere in the middle, over the age of 65 where risk/diagnosis of bone loss and osteoporosis often occurs, or a parent who can support the building of strong bones by guiding their children’s diets, this blog post will likely give everyone something to take away to build upon to support their bone health!
What is osteoporosis?
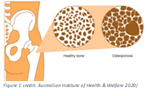
Osteoporosis is a condition resulting in ‘brittle’ bones – whereby the bones lose minerals leading to loss of bone density. As you can see in the picture, the bones look “spongey” or somewhat hollow, reflecting brittleness of the bones, causing them to be much more fragile and prone to breaking!
Osteoporotic fractures can result in reduced quality of life, reduced mobility, chronic pain, disability, increased risk of further fractures, and risk of mortality.
Am I at risk?
Did you know that by our late 20s we reach peak bone mass? This is why nutrition and exercise are so important growing up as the best initial way to support lifelong bone health – you can think of it as an investment for your future self!
As we age, (& especially during menopause in women) we lose bone density gradually. All of this is especially important to note, as once we have reached that peak, it is very difficult to meaningfully increase bone density! The best way after this phase of our life is to nourish ourselves in aim of maintaining the bone mass we have developed.
There are many risk factors for losing bone density. Some common examples include:
– family history
– hormonal changes (estrogen in females & testosterone in males)
– some medications
– smoking
– excessive alcohol intake
– excessive caffeine/coffee intake
– low physical activity level
– nutrition deficiencies / low intake of certain nutrients (calcium, exposure to vitamin D, protein intake, micronutrients)
The good news! You can manage your risk of developing osteoporosis, and support the maintenance of bone density, via lifestyle strategies.
Exercise! Another reason to love moving your body – getting active, and especially utilising resistance training, can help build peak bone density, and in older people prevent bone loss, by activating bone-building cells (called osteoblasts!). It has been found that people who are active in their daily lives can be up to 45% less likely to experience a hip fracture. Even jumping on a trampoline can be effective in stimulating bone growth! Another bonus of resistance exercise is building and maintenance of muscle – which contributes to strength, mobility, and balance (i.e. helps reduce risk of falling).
Lifestyle choices: if you are a smoker, consider reducing and quitting. Likewise, with alcohol intake; aim to stick to the national guidelines of no more than 2-4 standard drinks (or 10 standard drinks over 7 days) and aiming to have at least 2 alcohol free days per week
(here is the Australian dietary guidelines information on what a standard drink is – you may be surprised! https://www.eatforhealth.gov.au/food-essentials/fat-salt-sugars-and-alcohol/alcohol)
Vitamin D: this super-nutrient helps absorb the calcium we eat, regulates calcium levels in the body, and is also involved in the growth and maintenance of bone tissue. The best way to get Vitamin D is simply spending some time in the sun, as we make vitamin D when we are exposed to UVB rays. In South Australia, it is recommended that in order to get adequate vitamin D in sunnier months we spend a few minutes most days of the week in the sun, and in the colder winter months, we need to aim to spend a total of 2-3 hours per week outside in the sun. One of the best spots to absorb are our forearms! My favourite way to get some vitamin D is a morning walk in a t-shirt, spending my lunch break outside, and catching up with friends for a walk or coffee outside at a café. If you think you may not be getting enough vitamin D, it may be worth discussing with your GP who can check your levels and recommend a supplement if required.
Nutrition!
Our nutrition can play a vital role in prevention and management of osteoporosis.
Calcium: this is the most common mineral we associate with our bone health – we probably all grew up learning that drinking milk is good for our bones and teeth! And it is true, 99% of calcium found in our bodies is in our bones! Unfortunately, >50% of Australians do not obtain enough calcium through their diet…
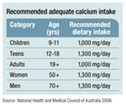
So, what foods have calcium, and how much should I eat?! The national guidelines recommend 1000mg-1300mg calcium dependent on age group. Calcium is found in a variety of foods. Dairy foods provide a dense source of calcium which is easily absorbable – e.g. milk, cheese, yoghurt, custard. Alternate dairy-free sources include tinned salmon/sardines with bones, calcium-set tofu, tahini (sesame seeds) and almonds, and some green veg/cabbage (however the calcium from these veggies is harder for us to absorb, and we need to eat much larger amounts to get a similar amount compared to dairy!). A dietitian can help with determining how much you need to include each day and assess your current dietary intake!
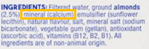
If you are someone who utilises plant ‘mylk’ or dairy free products – ensure you are choosing products that are fortified with calcium (check this on the ingredients label).
Protein: protein contributes to the bone-building process, maintenance of bone density, and muscle strength – which can complement resistance training and exercise to maintain good fitness, muscle mass and balance. Aim to include protein regularly throughout the day – a bonus is that dairy foods are good sources of protein so you get a double whammy!
Magnesium and Zinc: these minerals contribute to bone formation and preservation, and it isn’t uncommon for people to be deficient in these! Look to include leafy greens, nuts, seeds, wholegrains, legumes, dried fruit and meats/poultry/seafood (especially oysters!) for your mineral-fix.
Vitamin K: found in dark leafy greens and prunes, contributes to bone structure and density and is good to include in your diet. A bonus that these foods are dense in micronutrients and fibre which support overall health!
If you have been diagnosed with osteoporosis, osteopenia, vitamin/mineral deficiencies, have a family history of osteoporosis, or think that you could do with further support in improving your diet and lifestyle to support your bone health, we welcome you at Connect Healthcare! Our dietitian Tasha can provide you with individualised and tasty ideas to support your diet, and our group of movement-based practitioners can provide specialist advice on activity for supporting your bone health.
Resources
- https://www.osteoporosis.org.au/sites/default/files/files/Summary%20-%20Key%20Findings%20SA.pdf
- https://www.health.harvard.edu/staying-healthy/strength-training-builds-more-than-muscles
- https://www.osteoporosis.org.au/sites/default/files/files/OA%20Vit%20D%20Ed4.pdf
- https://www.osteoporosis.org.au/sites/default/files/files/ThematicReportSmaller.pdf
- https://www.osteoporosis.org.au/sites/default/files/files/OA%20Exercise%20Ed4.pdf http://www.scottsdalesportsmedicine.com/content/dexa-bone-density-scan
- https://www.osteoporosis.org.au/about-osteoporosis
- https://www.aihw.gov.au/reports/chronic-musculoskeletal-conditions/osteoporosis
- https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000333.pub2/full?highlightAbstract=osteoporosi%7Costeoporosis
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6323511/