By Scott Leslie
Lateral ankle sprains are one of the most common injuries sustained during sporting activities. For a lot of people, they seem to happen regularly, with little to no impact on their chosen activities. However, for some people these can lead to a diminished quality of life and physical activity, with the development of chronic ankle instability and an increased risk of ankle osteoarthritis (1).
Most athletes return to sport within 21 days, which is well before full ligament healing and recovery, and subsequently up to 70% of patients report a repeat of the injury within 12 months (1).
This therefore suggests that a thorough management and prevention of these injuries is very important.
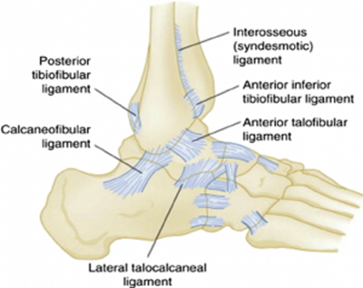
Anatomy
The main ligaments that stabilise the lateral (outside) ankle are the anterior talofibular ligament (ATFL), posterior talofibular ligament (PTFL), calcaneofibular ligament (CFL), lateral talocalcaneal ligament (LTCL).
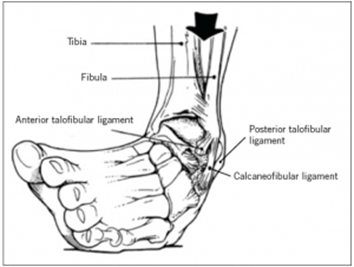
Mechanism of Injury
The lateral ligament structures of the foot are put under the most pressure, and likely to be injured when stress is placed on a Supinated (rolling the foot outwards) and Plantar-flexed (pointing the foot downwards) foot.
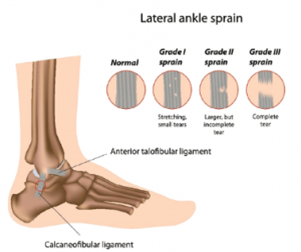
The extent of the injury to the ligaments are categorised as follows.
Ankle Sprain Grading Scale Proposed by Malliaropoulos et al. 2009
| Grade 1 | Grade 2 | Grade 3 |
| – No loss of function – No ligamentous laxity with anterior drawer and talar tilt testing – Little or no bruising – No point tenderness – Decreased total ankle motion of 5 degrees or less – Swelling of 0.5 cm or less as measured by figure-of- eight testing | – Some loss of function – Positive anterior drawer test, negative talar tilt test – Bruising – Point tenderness – Decreased total ankle motion > 5 degrees but < 10 degrees – Swelling > 0.5 cm but < 2.0 cm | – Near total loss of function – Positive anterior drawer and talar tilt test – Bruising – Extreme point tenderness – Decreased total ankle motion > 10 degrees – Swelling > 2.0 cm |
Management – Initial Phase
Like most soft tissue injuries, the immediate treatment for the ankle sprain is to follow the POLICE technique:
- Protection – limiting the stress on the injured ligament with a brace or protective taping.
- Optimal Loading – progressive loading of your injury can help promote optimal healing.
- Ice – Ice cools the tissue and can reduce pain, swelling and bleeding.
- Compression – limits the amount of swelling and stops internal bleeding.
- Elevation – helps to limit the bleeding and increases drainage of the swelling through the lymph vessels.
Management – Recovery Phase
The aim of the rehabilitation from a lateral ankle sprain is to allow healing of the ligaments, while also recovering full function of the joint. This includes the use of:
- Ankle Braces
- Joint Range of Motion
- Muscular Strength
- Balance
1. Ankle Braces
There is a predictable healing pathway for injured ligaments, and the ankle is no different to other ligaments in our body. The proliferative phase after ligament injury can last for weeks to several months during which time the healing ligament remains mechanically weak and subject to re-injury (2).
Therefore, ankle braces are advised for the initial 12 weeks, and are highly recommended when returning to sport for up to 6 months from the initial injury. By helping prevent the inversion action that causes the injury, it provides a better chance for the ligament to heal.
2. Range of Movement
Evidence suggests early mobilisation permitting the athlete to bear weight as tolerated for daily activities (functional mobilisation) is superior to prolonged rest in regards to time to return to work or sports, long-term ability to return to sports, persistent swelling, and long-term ankle instability (3).
Active, but gentle range of movement exercises for the ankle can be initiated as soon as pain tolerance will allow. This is predominantly in the ankle flexion range, as a lack of flexion can also be a predictor of future injury. We avoid inversion in the early phases to allow the ligaments to heal.
3. Strengthening Exercises
Strength begins with isometric exercises performed against an immovable object, again beginning with only flexion directions and adding inversion/eversion after.
This then progresses to dynamic resistance exercises using resistance bands. Toe curls, toe raises, heel walks, and toe walks may also be added to regain strength and coordination.
4. Proprioceptive and Balance Training
The aim is to develop strength and neuromuscular control so that the ankle and foot are better controlled and protected during stance and impact.
Once pain-free range of motion and weight bearing have been established, balance-training exercises should be incorporated (4).
A common progression when performing balance exercises is to move from double-leg stance to single-leg stance, eyes open to eyes closed, and firm surface to soft surface. Or beginning single leg balance activities eg. simple tasks like cleaning your teeth, progressing to throwing and catching a ball.
Returning to Activity
Medical specialists will use a series of tests that will ascertain your readiness for activity.
References
- Well B, Allen C, Deyle G, Croy T. Management of acute grade II lateral ankle sprain with an emphasis on ligament protection: a descriptive case series. Int J Sports Phys Ther. 2019;14(3):445-458.
- Cottrell JA, Turner JC, Arinzeh TL, O’Connor JP. The Biology of Bone and Ligament Healing. Foot Ankle Clin. 2016;21(4):739-761.
- Kerkhoffs GM, Rowe BH, Assendelft WJ, Kelly K, Struijs PA, and van Dijk CN: Immobilisation and functional treatment for acute lateral ankle ligament injuries in adults. Cochrane Database Syst Rev 2002.
- Mattacola CG, Dwyer MK. Rehabilitation of the Ankle After Acute Sprain or Chronic Instability. J Athl Train. 2002;37(4):413-429.
- Malliaropoulos N Ntessalen M Papacostas E Longo UG Maffulli N. Reinjury after acute lateral ankle sprains in elite track and field athletes. The American Journal of Sports Medicine. 2009;37(9):1755-1761.